When a child is diagnosed with a life-limiting or complex medical condition, families face an emotionally overwhelming and uncertain path. In these moments, pediatric palliative and hospice care can offer comfort, guidance, and meaningful support. Yet, many families are unfamiliar with what these services are—or worse, fear them due to common misconceptions.

Hospice vs. Serious Illness Care (Palliative Care): Understanding the Key Differences
Hospice vs. Serious Illness Care (Palliative Care): Understanding the Key Differences

When faced with a chronic illness, patients and their families often encounter terms like hospice and serious illness care (palliative care). While both are forms of care focused on comfort and quality of life, they have distinct purposes, goals, and timing. In this blog, we will dive into the differences between hospice and palliative care to help you understand how each approach can support you or a loved one during a challenging time.
What is Serious Illness Care (Palliative Care)?
Serious Illness Care is a specialized form of medical care aimed at improving the quality of life for people living with serious or chronic illnesses. It focuses on symptom management, pain relief related to the illness, and emotional support — all with the goal of making the patient feel as comfortable as possible, regardless of whether the illness is terminal or not.
Key Characteristics of Palliative Care
- For any stage of illness: Serious Illness Care can begin at any point during an illness, even when a patient is still undergoing curative treatment. It does not require a terminal diagnosis. Patients may continue with their primary treatments for their illness (like chemotherapy or surgery) while receiving palliative care.
- Symptom management: Serious Illness Care teams focus on alleviating physical symptoms such as pain related to the illness, nausea, fatigue, and difficulty breathing, as well as emotional symptoms like anxiety and depression.
- Skilled, Experienced Care Team: Serious Illness Care is interdisciplinary, meaning it involves a team of nurse practitioners and social workers who address the full spectrum of a patient’s needs. Lightways partners with the patient’s primary physician and/or other healthcare professionals involved in their care to provide another layer of support.
- Improving quality of life: The primary goal is not to cure illness but to improve the overall quality of life by managing symptoms and supporting the patient and their family.
Who Can Benefit from Serious Illness Care (Palliative Care)?
- Anyone with a serious illness like cancer, heart failure, COPD, kidney disease, or dementia.
- People are seeking relief from symptoms, even if their condition is not terminal.
- Families and caregivers who need emotional and psychological support.
What is Hospice Care?
Hospice care is specifically designed for patients who are nearing the end of life, typically when they are expected to live six months or less. The focus of hospice care shifts to comfort and dignity in the final stages of life, and it is provided when curative treatments are no longer an option or have been chosen to be discontinued.
Key Characteristics of Hospice Care
- End-of-life care: Hospice is for patients who are no longer pursuing curative treatments and whose illnesses are terminal. It focuses on comfort, pain management, and emotional support.
- Team-based care: Like palliative care, hospice involves a team of healthcare professionals — including doctors, nurse practitioners, nurses, social workers, nurses’ aides, integrative therapists, chaplains, and volunteers — who support both the patient and their family. The team works together to ensure patients are able to live life to the fullest possible.
- Home-based or inpatient options: While most hospice patients receive care at home, some may require inpatient care if their symptoms are more severe and need closer monitoring. Hospice services are provided wherever the patient considers their home, whether that’s their house, in a hospice facility, or in a nursing facility.
- Family support: Hospice care also provides dedicated support for family members, including education about how to provide care and what to expect, respite care, counseling, and grief support services before and after the patient’s death.
Who Can Benefit from Hospice Care?
- Patients who have a terminal illness and are expected to live six months or less.
- Patients who have decided to stop curative treatments and focus on comfort and quality of life.
- Families who need guidance, emotional support, and respite during a loved one’s final days.
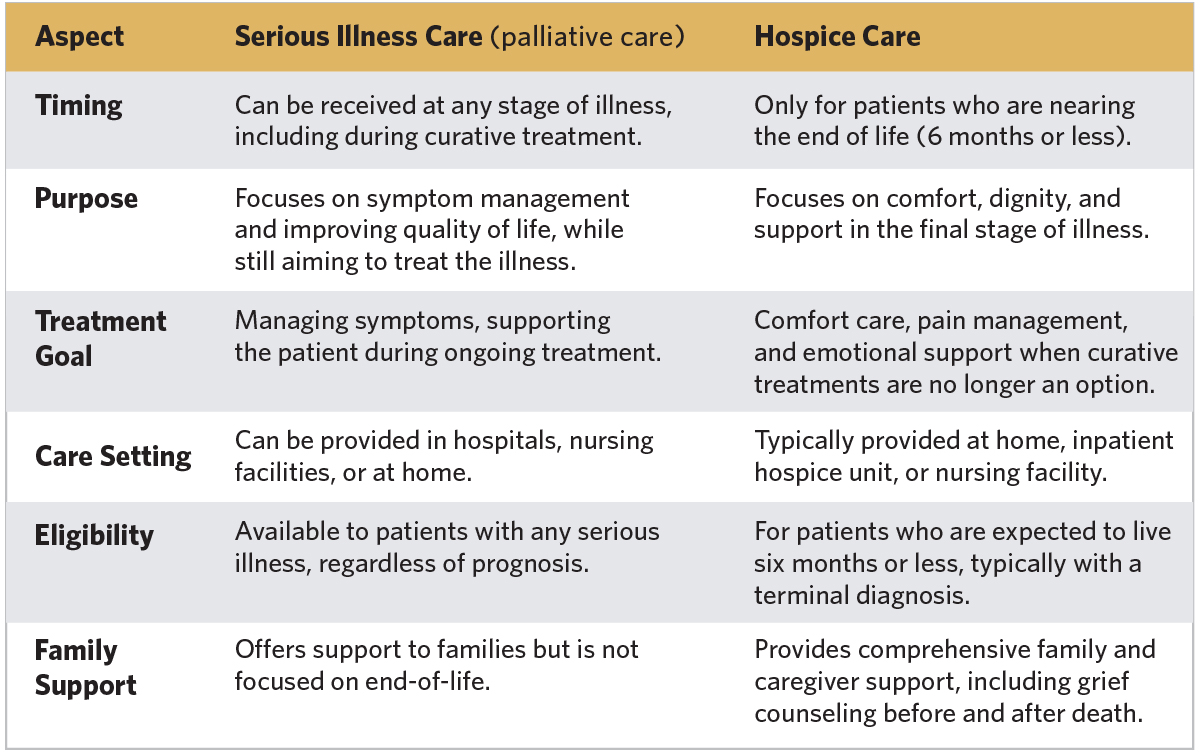
Key Differences Between Hospice and Palliative Care
Which Care is Right for You?
The choice between hospice and serious illness care (palliative care) depends on your loved one’s health status and goals. Serious Illness Care is a great option if you are looking for relief from symptoms but still wish to pursue curative treatment. It can be provided at any time during an illness. On the other hand, hospice care is designed for those whose focus shifts away from curing the illness and toward ensuring comfort and dignity in their final days.
Both forms of care aim to improve the patient’s quality of life, but hospice care is more focused on the end-of-life stage, while palliative care can begin earlier in a person’s illness journey. If you are unsure about which type of care is best, speak with your healthcare provider. They can guide you through your options based on your or your loved one’s specific needs. Or please call us and we can help you talk to your physician.
Understanding the difference between hospice and serious illness care can help you make an informed decision about the type of support you or your loved one needs. Whether you are seeking symptom relief during treatment or focusing on comfort and support during the final stages of life, both hospice and serious illness care are designed to ensure that patients receive the care they deserve — tailored to their individual needs and wishes.
Schedule a consultation
Contact Lightways Hospice and Serious Illness Care directly at 815.740.4104 for additional information or to schedule a consultation.